What to Know About Gynecological Cancers
Women can protect themselves from breast, cervical, ovarian and uterine cancers with regular screenings and self-monitoring.

Carmael Stagner, a single mother in Honolulu, was diagnosed two years ago with triple-negative breast cancer, an aggressive condition that required intensive treatments. What stunned her was how the cancer was found. During an annual wellness exam in October 2021, four months after a negative mammogram, Stagner’s physician felt a 3-centimeter lump in her right breast, even though “there were no symptoms, no pain, no discharge,” she says. “Had I done all the screening in June 2021, the lump would not have been found before it metastasized.”
Stagner underwent a full mastectomy, followed by 32 rounds of radiation and eight rounds of chemotherapy. Today, she feels stronger but needs two more years of quarterly blood tests and biannual infusions of a medication to reduce bone complications.
Joanne Hayashi of Honolulu had a similar diagnosis eight years ago in her early 30s: stage 3 triple-negative breast cancer. “I happened to come across a hard lump in my breast when I was rinsing off in the shower,” she says. Due to the large size of the tumor, Hayashi opted for a lumpectomy (partial removal of the breast), followed by radiation treatments.
She’s been cancer-free since 2016 and now serves as co-founder and president of the nonprofit advocacy and support group Breast Cancer Hawai‘i. “It’s very important for women to be vigilant about their health by getting regularly screened and making healthy lifestyle choices,” she says.
Breast cancer is one of four gynecological cancers that can be caught and treated early with routine screening. Here’s what women in Hawai‘i should know.

Breast Cancer
Breast cancer comprises 34% of cancers affecting women in Hawai‘i. Symptoms range from swollen lymph nodes and changes to the breast’s shape or texture to bloody discharge from the nipple.
Risks: Women with a family history of the disease, or hereditary breast and ovarian cancer syndromes, have a higher risk of developing breast cancer, says Ashley D. Marumoto, breast surgical oncologist at The Queen’s Medical Center. High-risk mammogram and MRI screenings are recommended for women who received thoracic radiation as children and those previously diagnosed with high-risk breast lesions.
Prevention and Screening: Women can self-monitor for breast lumps and abnormalities. Also, annual mammograms are recommended for women starting at age 40, a decade younger than the previous recommendation.
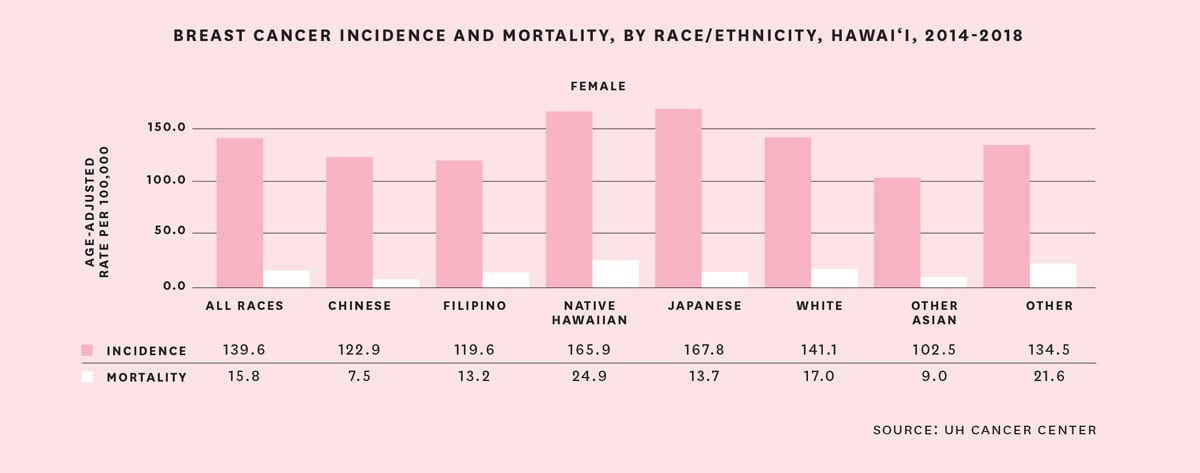
More females in the Islands are diagnosed with breast cancer (140 per 100,000 females) compared to the national average (128 per 100,000 females), according to the American Cancer Society. Additionally, women of Native Hawaiian and Japanese descent have higher incidences and mortality rates compared to women with Chinese, Filipino, other Asian and Caucasian backgrounds.
The good news is that Hawai‘i has one of the highest rates of breast cancer screening (83.7%) compared to the national average (78.3%).
“We know that if we screen more, we will detect more,” Marumoto says. Other factors, including lifestyle and genetics, could also explain the higher rate of breast cancer in Hawai‘i, she says. “This is being investigated in ongoing studies across the state.”

Cervical Cancer
When a woman’s cervix is infected with human papillomavirus, or HPV, it puts her at risk of developing cervical cancer. Symptoms include spotting or abnormal periods, bleeding and discharge, and pain during intercourse. Males and females can be asymptomatic carriers of the human papillomavirus and unknowingly infect their partners via skin-to-skin contact.
Risks: Smoking doubles the risk of cervical cancer because tobacco weakens the immune system and damages the DNA of cervix cells. Certain ethnic groups, such as Native Hawaiians and Pacific Islanders, have higher rates of cervical cancer compared to other populations, says Thanasak Sueblinvong, a gynecologic oncology specialist at Kaiser Permanente Hawai‘i. “Sometimes, there are cultural factors that prevent women from coming in to see a gynecologist,” he says. “We experience this more frequently with patients of Pacific Islander and Asian heritage.”
Prevention and Screening: Cervical cancer screening is recommended for women 21 through 65. The Pap smear and HPV test is done every three to five years. “HPV testing is now integrated into the Pap test for women who are 30 to 65 years old, which helps increase the sensitivity of cervical cancer screening in this age group,” Sueblinvong says.
Also, the HPV vaccine is recommended for children starting at age 9, before they become sexually active, and for adults up to age 26. Vaccinated women might think they don’t need cervical cancer screening as they get older, “but I want those women to know that while the HPV vaccine protects against the most common HPV strains that cause cervical cancer, the vaccine does not cover every type,” Sueblinvong says, “so cervical cancer screening is still necessary even for women who are vaccinated.”

Ovarian Cancer
Ovarian cancer is called “the silent killer” because symptoms aren’t always obvious or can mimic common illnesses. Women with ovarian cancer might feel persistent abdominal and pelvic pain, fatigue, bloating, constipation, urinary urgency, rashes, gas pains, appetite loss or feeling full quickly, irregular periods or painful intercourse.
“All women who experience symptoms, such as pelvic pain or pressure, or abdominal fullness or bloating, should be evaluated by their gynecologist or primary care physician, and an ultrasound of the pelvic organs will indicate if there are any concerns,” says Keith Y. Terada, gynecologic oncologist at The Queen’s Medical Center.
Risks: Family history is the single most important risk factor of ovarian cancer, says Michael E. Carney, gynecologic oncologist at Hawai‘i Pacific Health. The inherited genetic mutation in the BRCA1 and BRCA2 genes can increase the chance of developing the cancer by more than 50%. Also, white women who haven’t had children, or who have a history of breast cancer, are at greater risk. The odds, however, are lower for women who are on birth control pills or who have had their fallopian tubes tied or removed.
Prevention and Screening: Pelvic exams (included in women’s wellness exams) and imaging (such as a pelvic ultrasound) can detect cancerous abnormal growths in the ovaries. Another screening tool is the CA-125 blood test, which measures the amount of CA-125 protein in the blood. But it’s not as reliable as a stand-alone ovarian cancer screening tool, Carney says, “because half of early ovarian cancers and a quarter of advanced ovarian cancers have normal CA-125 levels.” Even men have some CA-125 in the body. The CA-125 blood test usually is given to women already diagnosed with ovarian cancer to measure and monitor protein levels during and after cancer treatments.

Uterine Cancer
Uterine cancer occurs when abnormal cells invade the lining of the uterus, also known as the endometrium. Symptoms of uterine cancer include irregular spotting and abnormal bleeding, discharge and pelvic pain.
Risks: Obesity is a major risk for uterine cancer because body fat converts to the hormone estrogen, and “too much estrogen can cause the lining of the uterus to grow too much, which can then increase the risk of uterine cancer,” says Paula Lee, gynecologic oncologist at Hawai‘i Pacific Health.
Some drugs (tamoxifen, for example, which is used to treat breast cancer and irregular bleeding) have been known to increase a woman’s risk of uterine cancer. And hormone supplements (estrogen-only pills without progesterone, for example) can increase risks, as well.
Prevention and Screening: Unlike mammograms and Pap smears, there is no regular screening for uterine cancer. The key is to maintain a healthy weight and body mass index and watch for symptoms (including unusual discharge from the vagina, pelvic pain or pressure, back pain, pain during intercourse and pain during urination). Lee says she’s witnessed more cases of advanced uterine cancers in Hawai‘i than anywhere else, possibly “due to challenges in access to timely care and/or patients not knowing they need prompt medical evaluation.”
Late-stage uterine cancers are more difficult to treat and require multimodal therapy—surgery, chemotherapy, radiation and immunotherapy. Uterine cancers usually occur after age 55, but younger women should seek medical advice if they have irregular bleeding, are obese, or have genetic predispositions (family members with Lynch syndrome and cancers of the stomach, uterus, ovaries, colon and stomach).