The Marvelous Microbiome
A healthy gut is the core of good health.
“There are examples where manipulating the microbiome can solve human diseases.”
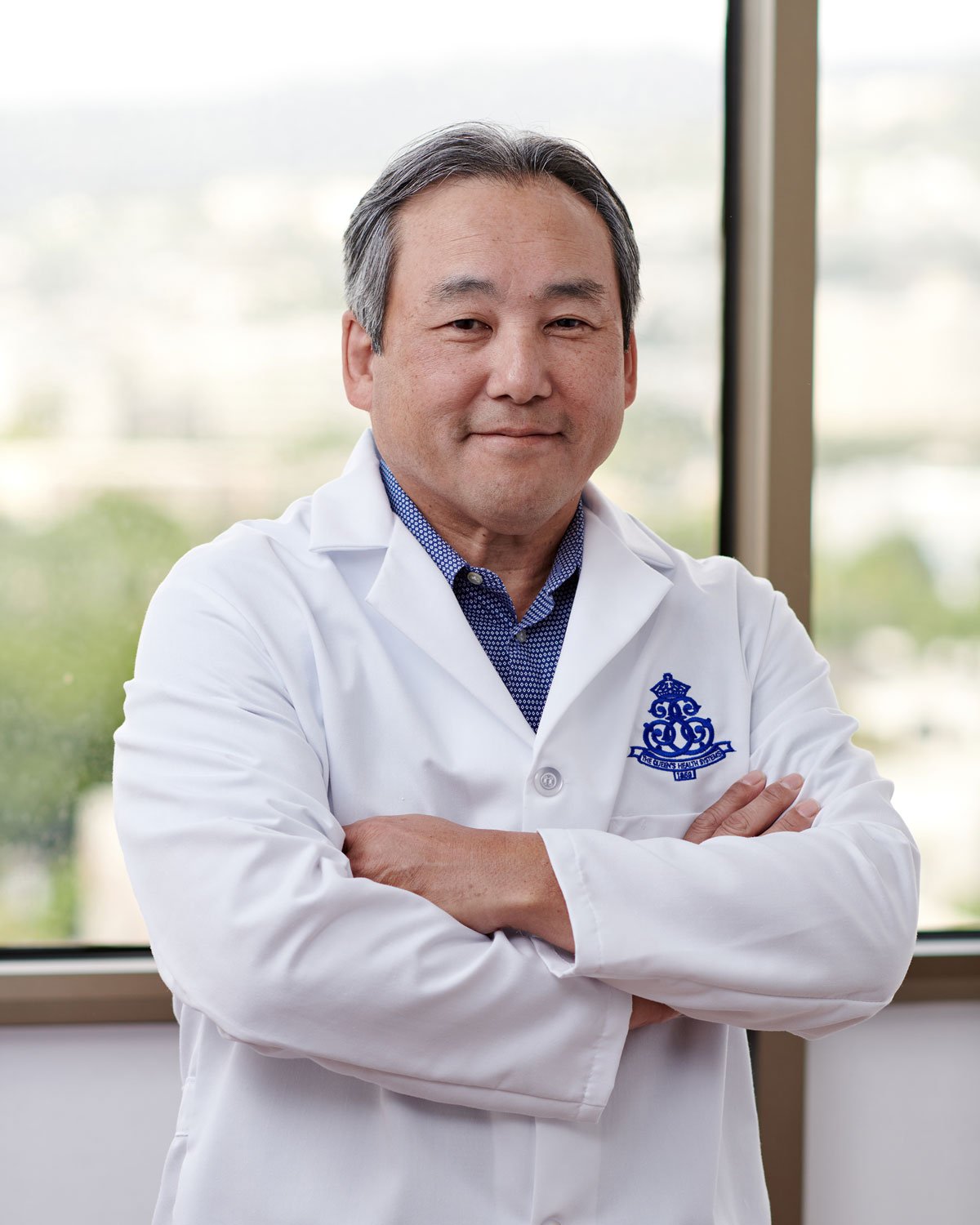
— Dr. Scott Kuwada, chief of gastroenterology at The Queen’s Medical Center and chair of medicine at the John A. Burns School of Medicine.
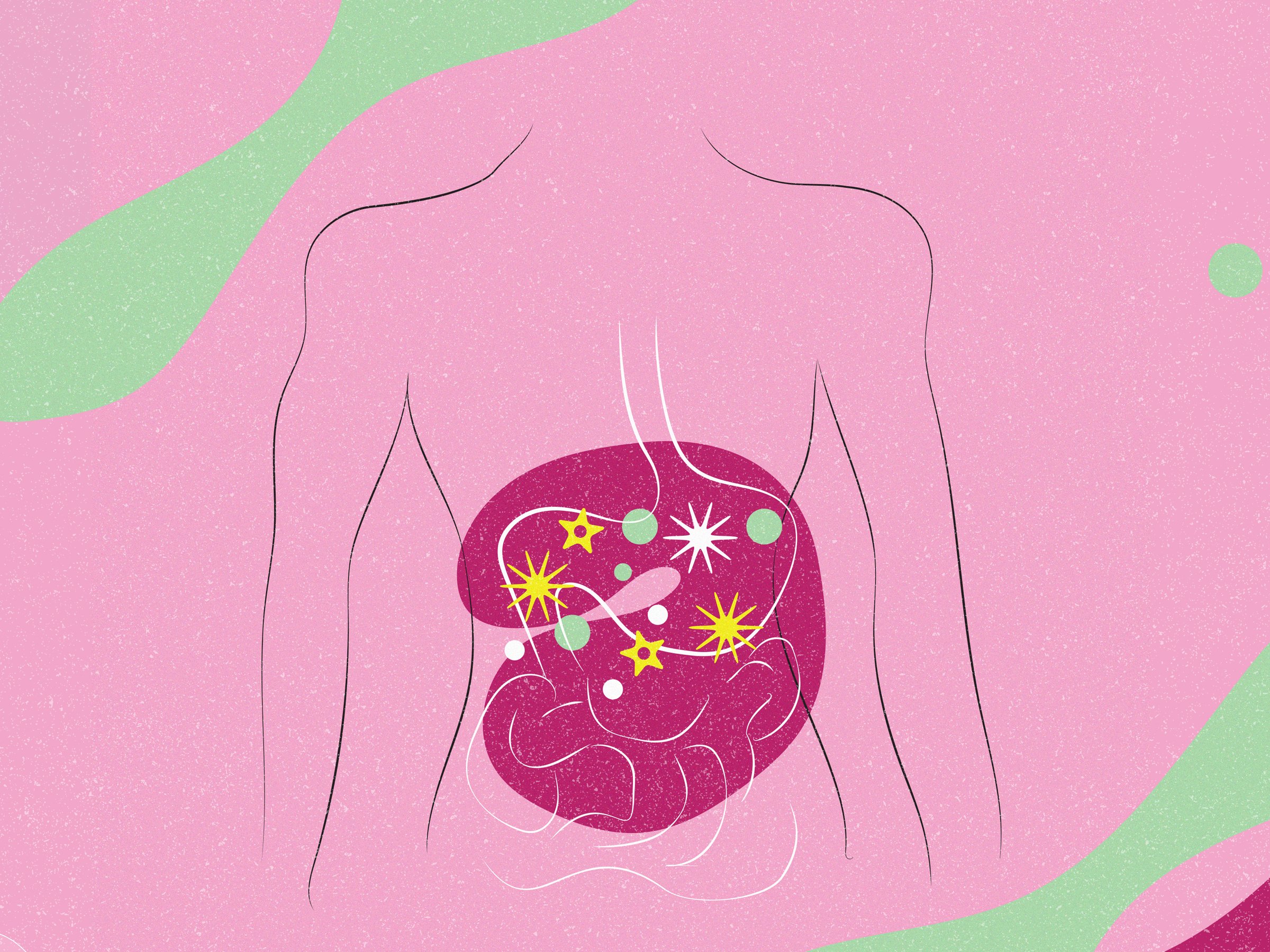
Who would have thought a word like “microbiome” would become so buzzy? But as researchers continue to connect the gut to the functioning of the entire body, nurturing a healthy gut microbiome has become a coveted pursuit.
Anyone who’s stayed abreast of health news knows the gut is far more than just an organ for digestion. It’s now deemed the body’s second brain, affecting everything from the immune system, skin, mental health and more. Medical researchers have linked it to diabetes, various cancers and autoimmune diseases, anxiety and depression, and most recently, Parkinson’s disease.
“The gut is an incredibly important gateway that’s exposed to what’s outside us, the environment,” says Dr. Scott Kuwada, chief of gastroenterology at The Queen’s Medical Center and chair of medicine at the John A. Burns School of Medicine.
The gut microbiome comprises trillions of microorganisms, namely bacteria, fungi and viruses. Scientists have learned it includes both harmful and beneficial microbes and bacteria, and that cultivating a healthy microbiome with so-called good bacteria is critical. “They play a very vital role, especially in regulating our immune responses to the environment,” Kuwada says.
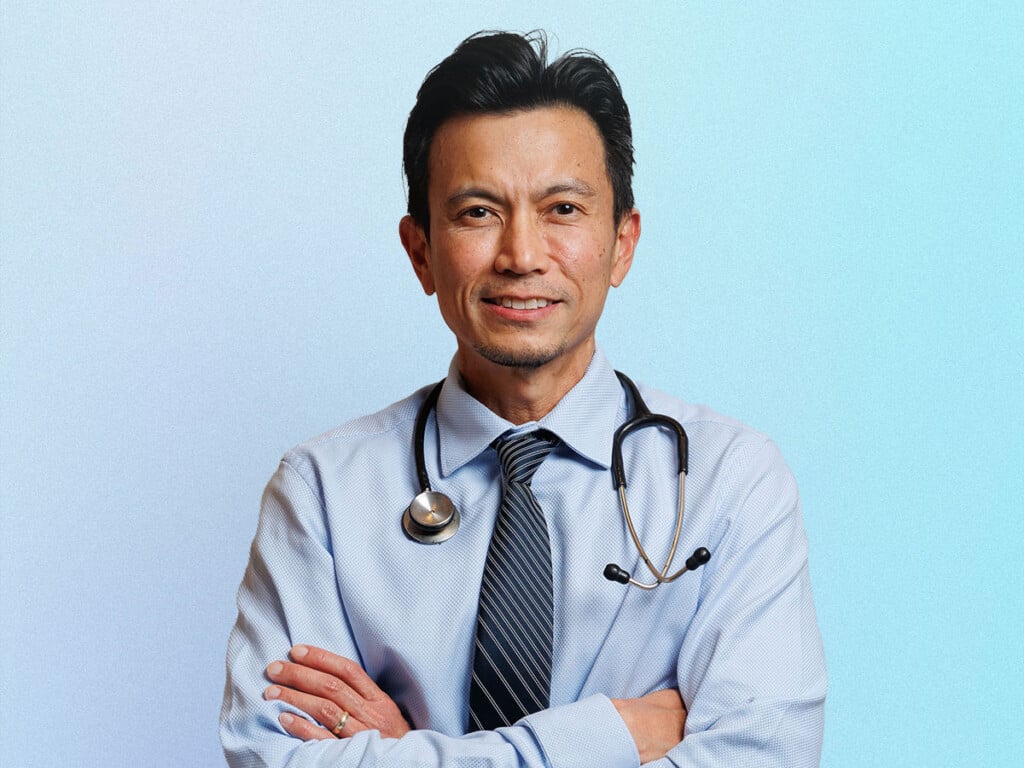
Adds Sara Chong, a functional medicine chiropractor in Honolulu who specializes in gut health: “I always tell my patients that once we understand what their microbiome looks like through gut testing, we can see whether there are too many bacteria and microbes that are toxic and causing inflammation. We then work with them to nourish the beneficial kinds that keep everything in check.”
The Mission: A Healthy Gut
As findings from microbiome research continue to make headlines, many people have embarked on gut-healing quests. After all, nearly two out of three adults are burdened by GI symptoms, according to a National Institutes of Health study. Some are visiting medical doctors like Kuwada, while others are seeking out functional medicine specialists like Chong. Still others are doing their own research, changing their diets, taking supplements and more.
As such, there are countless gut-enhancing products available, making it difficult to discern which ones may be helpful and which to avoid. I’m personally targeted for all this. Perhaps, my own mission to fix my gut embodies what others might be facing on their wellness journeys.
My Father’s Gut Woes
My father died of Stage 4 gastric cancer in 2011. He also had colon cancer at the time. When I was growing up, he battled a separate case of gastric cancer that had been deemed terminal. Although he defied the prognosis and survived, he struggled for the rest of his life with stomach issues, including ulcers, intestinal blockages, you name it. He popped antacids like they were mints. And although he was not a complainer, I could tell he suffered—a lot.
When I reached middle age, I started having gut-related issues of my own, which resulted in frequent stomachaches, constipation, bloating, feeling unwell after meals, hives, overall fatigue and malaise. My doctor was concerned because of the hereditary links of gastric cancer and advised me to undergo both a colonoscopy and stomach scope while in my 40s. Although both were clear, with the exception of gastritis (inflammation of the stomach lining), I didn’t feel well.
As years went on and my symptoms persisted, I finally got serious about repairing my gut. I dug into the research, reading scientific studies, books and articles. I watched Netflix documentaries and even took an online class on MasterClass, lured by its teaser: “Your gut is the gateway to great health. The world’s leading gut health experts teach how to boost well-being, starting with what’s inside you.” Although I’ve never done microbiome testing, I leaned into suggested recommendations to improve it—taking probiotics and prebiotics, eating fermented foods, avoiding antibiotics when possible and more.
I didn’t see marked improvements until this year, when I radically changed my diet. I stopped drinking alcohol and cut out red meat and all processed meats along with sugary sodas and artificial sweeteners. I now eat fresh vegetables, fruits and other whole foods at almost every meal and avoid ultra-processed foods and foods that are too spicy, as best I can.
The result: No more digestive issues, tiredness or hives—or any debilitating symptoms at all. I’ve become a true believer that good nutrition—along with other healthy habits—can heal, and that having a healthy microbiome is vital.
Until recently, it seemed weird to tell others about my experiences. I still get blank stares when I do, but after interviewing Kuwada, one of our state’s leading gastroenterologists, and Chong, I’m convinced balancing the microbiome is not just a health fad—it’s one of the pillars of health.
Fecal Transplants May Sound Weird
As more is discovered about the microbiome, innovative treatments continue to roll out, including in Hawai‘i. Kuwada says one of the relatively newer treatments involves a fecal transplant. “The million-dollar question is if you change somebody’s microbiome to look more like a healthy patient’s microbiome, what improvements in health do you get from that?” he says. “There are examples where manipulating the microbiome can solve human diseases.”
Fecal transplants have proven to be particularly beneficial for those with Clostridioides difficile—bacteria that Kuwada describes as “opportunists that can take over when they start multiplying,” causing severe intestinal inflammation when they’re not kept in check by other parts of the microbiome. “C. diff,” as it’s commonly called, can be found in feces and be contracted by coming into contact with contaminated surfaces.
In the past, patients were treated with antibiotics, but sometimes the infection returned, he adds. “We’ve now learned that the fecal microbe mycobacterial transplant, which is taking stool from a healthy donor, encapsulating it and having the patient swallow the capsules, has more than a 90% success rate in treating this condition. It may sound disgusting, but it’s been very successful.”
There are other examples where manipulating the microbiome is proving effective, including for ulcerative colitis, Kuwada says. In fact, he believes altering a patient’s microbiome could potentially address a lot of health conditions, including severe diseases.
He cites the link between the common bacteria Helicobacter pylori and cancer, for example. Helicobacter pylori is often caused by ingesting contaminated food or water. Those living in crowded areas with poor sanitation are more likely to get infected.
“It’s probably what caused your father’s stomach cancer,” Kuwada tells me of my dad, originally from North Korea. “I got into this field because one of my grandfathers had gastric cancer, and the other had colon cancer. With gastric cancer, there’s no question Helicobacter pylori is a major risk factor. The World Health Organization lists it as a group one carcinogen now. And we know immigrants coming to Hawai‘i from East Asia and the South Pacific have a much higher infection rate of Helicobacter pylori, and that we see a lot more gastric cancer in Hawai‘i than in other states. This research has changed our practices as gastroenterologists here—we now look for that infection.”
As research deepens, we’ll learn more about which bacteria are beneficial, and how our microbiomes could be altered to include these types of bacteria to halt or prevent diseases, Kuwada says. “Again, those are $10 million questions that are still being discovered.”
SEE ALSO: Gut Instincts

10 Tips to Improve Your Microbiome
Courtesy of Sara Chong, a functional medicine chiropractor specializing in gut health.
- Eat a diverse range of foods full of colorful fibrous veggies/fruits.
- Add fermented foods: kim chee, yogurt, sauerkraut, pickles, miso, etc.
- Take quality probiotics to improve digestion, lower inflammation and support immune health.
- Drink plenty of water to increase the protective mucosal gut lining and benefit healthy gut bacteria.
- Eat fiber-rich foods like garlic, asparagus, leeks and bananas.
- Eat polyphenol-rich foods, including dark chocolate, berries and olives, and drink green tea, also rich in polyphenols.
- Avoid antibiotics, alcohol and processed foods, all of which directly damage/destroy gut bacteria.
- Manage stress, which increases inflammatory gut bacteria.
- Get quality sleep. Studies show that even one sleepless night can change the quality of gut bacteria. That bacteria can go from healthy and beneficial to the kind that increases inflammation and obesity overnight.
- Exercise regularly. Moderate exercise improves gut microbiome diversity.